Introduction
Bone healing is a remarkable biological process that repairs fractures and restores strength. Whether you’ve suffered a minor crack or a complex break, understanding bone structure and healing phases can help you optimize recovery.

This guide covers:
✔ Bone anatomy (cortical vs. trabecular bone)
✔ Perren’s Strain Theory – why movement affects healing
✔ The 4 stages of secondary bone healing
✔ Primary vs. secondary healing (and when each occurs)
✔ How doctors assess fracture union
1. Bone Anatomy: Cortical vs. Trabecular Structure
Bones are not just solid structures—they have a complex, dynamic architecture that influences healing.
Cortical Bone (Compact Bone)
- Made of tightly packed osteons (Haversian systems).
- Contains central Haversian canals (blood vessels) surrounded by concentric lamellae.
- Volkmann’s canals connect osteons for nutrient exchange.
- Found in diaphyses (shafts) of long bones, providing strength and rigidity.
Trabecular (Cancellous) Bone
- Spongy, porous structure with woven trabeculae.
- Found in metaphyses (ends of bones) and vertebrae.
- Provides shock absorption and supports bone marrow.
🔗 Learn more about bone anatomy from the NIH Osteoporosis Resource Center.
2. How Do Bones Heal? Perren’s Strain Theory
Fracture healing depends on mechanical strain (movement at the break site).
- >10% strain → Forms granulation tissue (no bone growth).
- 2-10% strain → Forms fibrous tissue (scar-like).
- <2% strain → Allows bone formation (optimal healing).
This explains why:
✔ Stable fractures (minimal movement) heal faster.
✔ Unstable fractures (high strain) may need surgical fixation.
3. The 4 Stages of Secondary Bone Healing (Callus Formation)
Most fractures heal through secondary healing, involving four key phases:
First Phase: Inflammation (Week 1)
- Haematoma forms at fracture site.
- Immune cells (neutrophils, macrophages) remove debris.
- Symptoms: Swelling, heat, pain, redness (rubor, calor, tumor, dolor).
2nd Phase: Soft Callus (Weeks 2-3)
- Fibrous tissue & cartilage replace granulation tissue.
- Fracture becomes “sticky”—resists shortening but not bending.
- X-rays may show widened fracture gap (due to bone resorption).
3rd Phase: Hard Callus (Weeks 4-12)
- Osteoblasts form woven bone (visible on X-rays).
- Healing methods:
- Intramembranous ossification (direct bone formation under periosteum).
- Endochondral ossification (cartilage → bone transformation).
- Fracture becomes rigid but not fully strong.
4th Phase: Remodeling (Months to Years)
- Woven bone → Lamellar bone (stronger, organized).
- Follows Wolff’s Law: Bone density increases where stress is highest.
- In children, bones fully remodel; in adults, some deformity may remain.
🔗 Explore fracture healing timelines at OrthoInfo.
4. Primary Bone Healing (Direct Healing Without Callus)
Occurs only with rigid fixation (e.g., plates & screws).
- No callus forms—bone heals directly via osteoclast/osteoblast activity.
- Cutting cone mechanism: Osteoclasts tunnel, osteoblasts lay new bone.
- Slower than secondary healing but avoids soft callus weakness.
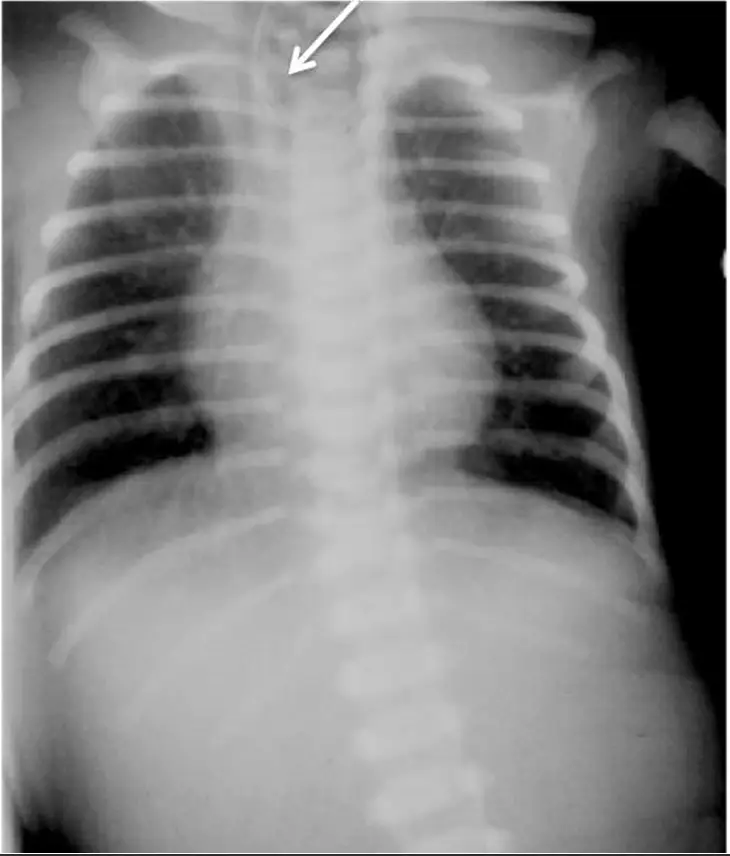
5. How Do Orthopedics Know If a Fracture Is Healed?
Healing is confirmed by:
✅ No pain on weight-bearing
✅ No tenderness or abnormal movement
✅ X-ray signs:
- 3/4 cortices bridged (long bones).
- Bridging trabeculae (metaphyseal fractures).
Conclusion
Bone healing is a complex but fascinating process influenced by strain, stability, and biology. While secondary healing (callus formation) is most common, primary healing ensures precision in surgically fixed fractures.
Key takeaways:
✔ Movement affects healing (Perren’s Strain Theory).
✔ Secondary healing has 4 stages (inflammation → remodeling).
✔ Rigid fixation enables primary healing (no callus).
✔ Full remodeling can take years, especially in adults.
🔗 For more on bone health, visit Mayo Clinic’s Orthopedic Guide.
Also read: Fracture assessment and fracture radiological assessement